Giving report is a part of every nurse’s daily routine.
It is a way to communicate crucial information during shift changes and patient transfers quickly.
This step-by-step tutorial will help you perform this critical skill more effectively for continuous, high-quality patient care.
Why is Giving a Good Handoff Report Important?
A good handoff report sets nurses up for success. A focused, concise report provides the information you need to plan your shift. It is easy to understand the patient’s condition and plan care when report is well organized.
Since care planning entails how you treat each patient and in what order, a good report boosts your performance.
Giving Report That Supports Other Nurses

Whether you’re the off going nurse or transferring a patient to another unit or setting, giving a report is crucial for ensuring the patient receives all the medications, treatments, and general care they need.
While the personalities and working styles of nurses vary considerably, care should be consistent across staffing or setting changes.
No matter which setting you’re in, you need to be on time and ready to focus during report fully.
Whether your facility does report at the bedside, breakroom, or a corner of the nurses’ station, during report the oncoming nurse receives enough information to render care safely.
Diligent and conscientious care is one of the main reasons most people see nurses as extremely trustworthy.
What To Include in the Nurse’s Report
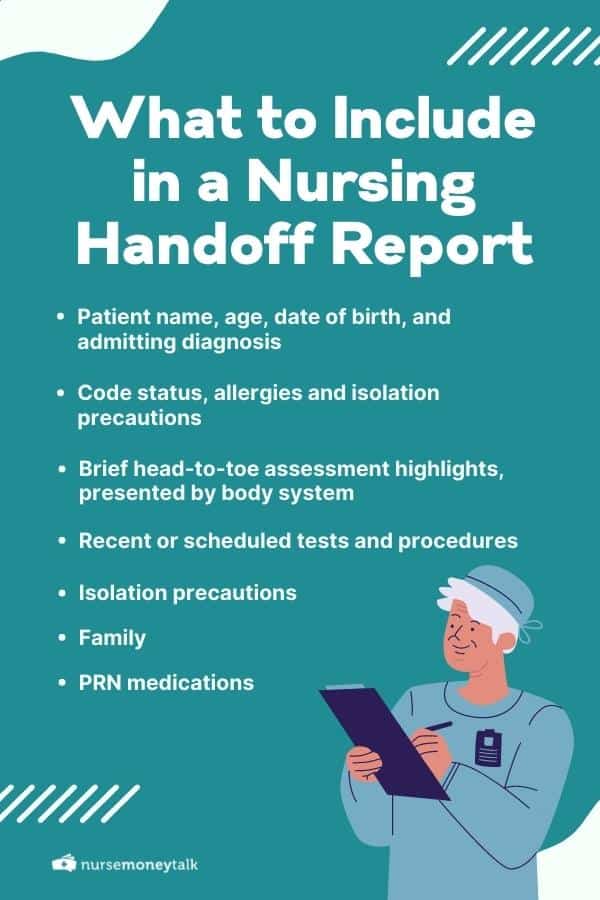
The worst mistake nurses cite regarding report is leaving out important information, such as upcoming tests and procedures.
Since these procedures frequently happen early in the shift, knowing they are scheduled gives you a chance to design care so that the patient is ready to go when transport arrives.
When giving report, it is essential to remember that you’re giving a brief introduction or update to the oncoming nurse.
While you can include critical lab results or medication changes, there is no need to read off a list of these items since they’re easy to look up on the computer.
The same is true for comorbidities. Unless comorbidity directly impacts their care, there is no need to share it in report.
Some items that you need to include are:
1. Introducing the Patient
After briefly introducing the patient, please share any allergies and their code status.
When you list their code status, it’s also a good idea to remind the oncoming nurse to refer to their chart for their living will or POLST (Physician’s Orders for Life-Sustaining Treatment).
Isolation precautions have taken on increased importance in recent years due to the COVID-19 pandemic.
While we must limit the spread of coronavirus, we also must do our best to protect others from MRSA, RSV, and other infections by maintaining contact, airborne, or droplet precautions.
2. Systems Overview
Once you’ve shared their doctor and any consults you may have out for the patient, you can begin sharing any pertinent assessment data, including any relevant vital signs.
Since assessments are typically conducted using a head-to-toe or systems approach, report should be shared using one of these formats.
Lungs
Begin with breath sounds. State that their lungs were clear or describe any adventitious breath sounds, such as crackles, along with the lobe in which you heard them.
Relay how many liters of oxygen they are on and if it is being delivered by nasal cannula, nonrebreather, or other system. Describe their cardiac sounds and share if they’re on telemetry.
Neuro Status
Reveal their neuro status and if they’re alerted and oriented times four, as well as if they’re confused, pleasant, or display challenging behavior.
Alert the oncoming nurse to any hearing aids, glasses, and other assistive devices. It’s also a good idea to share if they move independently or require the assistance of at least two, three, or more staff members.
GI/GU
Detail their gastrointestinal and urinary function, including bowel sounds, time of last bowel movement, and any urinary or fecal incontinence.
Relay complaints of nausea, vomiting, and diarrhea, including what measures you’ve taken to help alleviate them.
Hydration and nutritional status are essential to share, including whether they are on thickened liquids, low sodium, or any other special diet.
If they have a PICC, peripheral, or central line, list any fluids or medications running through it.
If they have diabetes, share their renal status, including relevant labs and blood glucose values.
Skin
Describing their skin is very important.
Please include any wounds as well as dressing changes, wound vac, or other care the oncoming nurse needs to perform during their shift.
3. Future Planning Considerations
Notify the oncoming nurse of any scheduled procedures and tests for their shift so they can have the patient ready for them.
List any patients who are NPO (nothing by mouth) so that they can ensure the patient doesn’t receive a breakfast tray or intercept dietetics staff at their door.
If they have family in the room, please give the oncoming nurse a bit of information about them.
Some families prefer to perform some of the care, such as helping their family member wash their face or shave in the morning. Others prefer to leave such personal care to the staff. Knowing a family’s preferences can help prevent misunderstandings.
Sometimes, family members try to sneak in a few “forbidden foods,” so warning the oncoming nurse will help them be more alert to gently remind the family about their loved one’s prescribed diet.
Be sure to pass along any information about antibiotics and pain medication. Include their last dose and the time of their next dose, if applicable.
Pain management is critically important, and you should always share as much as possible about their pain level, quality of pain, and response to pain medication.
SBAR and iSoBAR
There are many ways to organize your thoughts during report. SBAR stands for Situation, Background, Assessment, and Recommendation.
Since it was invented by the rapid response team at Kaiser Permanente in Colorado in 2002, SBAR has been the standard for organizing report.
Using SBAR, you begin by briefly overviewing the patient and situation. Next, you give their background by describing the patient and what brings them to your facility.
Then, share your physical assessment of them and any vital test results. The recommendation section details your recommended plan of care, such as any doses of PRN medications, breathing treatments, or getting the patient ready for discharge in the afternoon.
iSoBAR is a newer reporting tool devised by the Western Australian Health Committee in 2009.
It adds information to the traditional SBAR format and clarifies the responsible parties during patient handoff.
iSoBAR is an acronym for Identify, Situation, Observation, Background, Agreed plan, and Read back.
Identify refers to providing basic information about the patient. Situation is the reason for continued care.
Observation is for sharing your head-to-toe or systems-based physical assessment and any recent data, such as vital signs or blood glucose levels.
Background is another word for their medical history, including allergies and code status. Agreed plan includes what needs to be done during the next shift.
Read back involves clarifying the report, identifying who the oncoming nurse is, and giving the oncoming nurse a chance to view the electronic medical record and ask any questions of the off-going nurse.
ISoBAR and SBAR Are Both Useful
Both SBAR and iSoBAR are helpful tools for organizing report and planning care.
iSoBAR has the advantage of including more patient information and specifying the identity of the oncoming nurse.
Research has revealed that iSoBAR is helpful for bolstering teamwork and communication among PACU (post-anesthesia care unit) nurses.
Boost Your Handoff Report Skills
No matter your setting, providing a good report can help the oncoming nurse more efficiently plan care.
Comment here with tips and tricks for giving report, or take a moment to find inspiration from other nurses.